Kei Owada, The University of Queensland; Ben Hayes, The University of Queensland; Ricardo J. Soares Magalhaes, The University of Queensland, and Timothy J. Mahony, The University of Queensland
Australian authorities are on high alert amid the spread of lumpy skin disease in cattle and buffalo across South-East Asia. While Australia remains free of the disease, the virus is likely to breach our borders at some stage.
Detection of the disease in Australia’s livestock industries would lead to restrictions on cattle, meat and dairy exports, with serious consequences for the economy.
The federal government has a plan to detect and respond to an outbreak. But we need to go one better – to predict where the disease is likely to appear and how it might spread.
Our team is developing a model we hope will provide this vital information. It will help Australia prepare and respond not just to the current threat, but to any future biosecurity breach.
What is lumpy skin disease?
Lumpy skin disease is a viral disease that affects cattle and buffalo, not humans. The incubation period is up to 28 days.
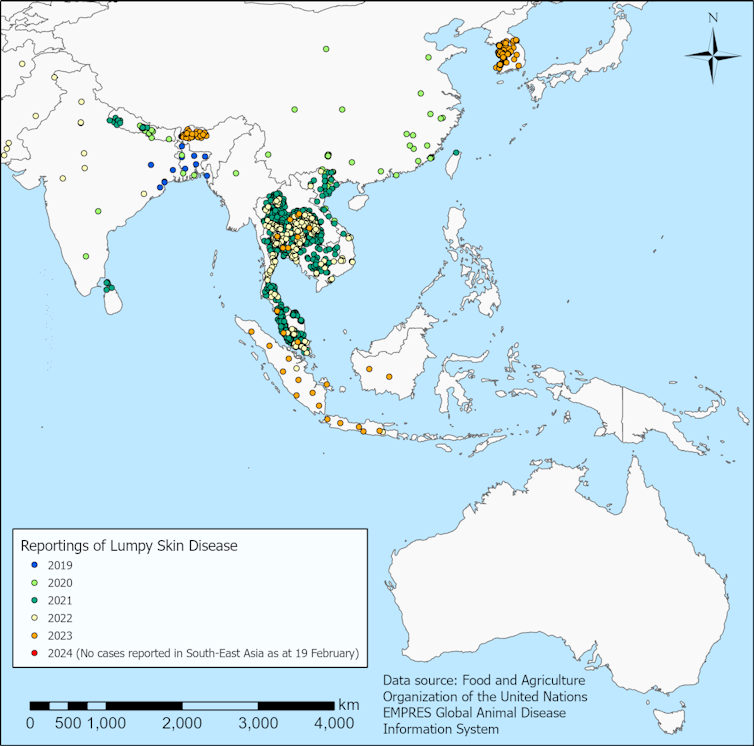
First reported in Zambia in 1929, the disease has spread across Africa, the Middle East, Eastern Europe and Asia. It reached Indonesia in 2022.
Early symptoms include fever and increased tear production. Lumps then appear on the skin and can cover the entire body, gradually hardening as the disease develops. Sometimes the lumps slough off, leaving holes on the skin that are susceptible to infections.
Typically only 1-5% of cattle die from the disease, but those that recover may not return to full health.
Milk production is reduced in cows. Meat yield from infected cattle is likely to be reduced, although it does not contain lumps and is safe to eat. Temporary or permanent infertility in both cows and bulls can also develop during the first month of infection.
The virus is mainly spread by biting insects such as mosquitoes, stable flies and ticks. Higher temperature and increased rainfall can increase insect populations and activity, and have triggered outbreaks of disease overseas.
The disease can also be transmitted by close contact between cattle, such as exposure to body fluids.
A testing time with Indonesia and Malaysia
In July last year, Indonesian authorities claimed 13 cows from Australia had tested positive days after arrival. At the time, Australian authorities demonstrated that the nation was free of the disease.
Nonetheless, trade between Indonesia and four of Australia’s cattle export holding yards was suspended immediately. Then Malaysia went further and stopped accepting any Australian live cattle and buffalo.
Malaysia and Indonesia each lifted their restrictions in early September, after more than 1,000 cattle were tested across Western Australia, Queensland and the Northern Territory. The Australian government also agreed to boost surveillance and biosecurity measures, including testing on farms and disinfecting departing export vessels.
Since the lifting of restrictions, the Indonesian government has reportedly rejected Australian cattle with skin blemishes – in some cases, this comprised up to 30% of cattle in a shipment.
How could lumpy skin disease enter Australia?
The Australian government has introduced strict biosecurity measures at international ports to minimise the risk of infected animals entering the country. These include disinfection and disinsection (spraying to remove insects) of vessels and cargo.
However, there’s a high risk of infected insects entering Australia through international ports or by travelling across the sea to northern Australia. Some infected flying insects may be able to cover long distances, aided by strong winds.
Another possible mode of entry for infected insects is through illegal fishers landing on the Australian coast.
What can be done to prevent the spread of lumpy skin disease?
In countries where lumpy skin disease is common, live vaccines have been used to control the disease. However, this is not practical in disease-free countries such as Australia, because vaccinated animals cannot be distinguished from infected animals. This means Australia could not be confirmed free of disease, leading to international trade restrictions.
The Australian government secured a supply of lumpy skin disease vaccines in October. These are being securely stored overseas in case of an outbreak. The vaccines will also be available to neighbouring Papua New Guinea and Timor-Leste.
Preventing the spread of lumpy skin disease requires early detection of the disease, isolation of potentially infected animals and restrictions around their movement. Once initial diagnosis is confirmed, culling of infected animals and insect control would likely follow.
What can be done to prepare Australia?
Australia has a veterinary emergency response plan to enact if the disease enters the country. The federal government has also boosted surveillance and begun offering training for veterinarians, industry and government staff on how to prevent and control the spread of the disease.
However, innovative models are needed to assess the likely introduction and spread of the disease in Australia. Our team is developing a framework to carry out such modelling. Our model will include data describing the current status of reports of the disease outside of Australia, Australia’s landscape and climate, distribution and movement of cattle, and local insect populations.
These models will produce maps that can be used to identify areas in Australia more suitable to receiving the disease, such as areas with favourable environmental conditions for the survival of imported infected insects. These maps will inform decisions around surveillance and response plans, and help farmers prepare for a potential outbreak of the disease.
Maintaining a high level of preparedness and awareness of the disease among cattle producers, farmers, veterinarians and other relevant individuals is paramount if we are to maintain our disease-free status as an international exporter. ![]()
Kei Owada, Postdoctoral Research Fellow, The University of Queensland; Ben Hayes, Director, Centre of Animal Science, University of Queensland, The University of Queensland; Ricardo J. Soares Magalhaes, Professor, The University of Queensland, and Timothy J. Mahony, Professor, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.



